THE ROLE OF ECHO
Echo is not sensitive enough to rule out pulmonary hypertension associated with interstitial lung disease (PH-ILD)2-4
In a cohort of patients with ILD clinically suspected of having PH-ILD* (N=265)
40%
of patients with an echo showing a low likelihood of PH were confirmed to have PH-ILD by RHC3*†
| Echo probability of PH† | Patients, n |
Patients with PH, n (%) (confirmed by RHC) |
|---|---|---|
|
Low |
43 |
17 (40%) |
|
Intermediate |
60 |
42 (70%) |
|
High |
162 |
135 (83%) |
Low probability of PH was defined as TRV ≤2.8 m/s or unmeasurable, with no other echo signs of PH.3
Do not rely on echo alone to detect PH. Incorporate worsening clinical symptoms and routine ILD test results into your PH detection strategy.2-4
Why does echo have limitations for identifying PH early?
Echo findings alone do not always detect early-stage PH.5-7
- Signs of RV dysfunction appear in later-stage PH
- Some echo findings that are suggestive of PH require expert echo assessment and may not be routinely evaluated
RVSP estimates of mPAP derived from echo are frequently inaccurate or not reported.2,4-6,8
In fact, in about 50% of patients with ILD, TR jet velocity (used to calculate RVSP) may:
- Frequently over- or underestimate RVSP, causing echo estimates to differ from RHC values by >10 mm Hg†
- Be difficult to visualize, preventing RVSP from being calculated or reported
Echo is just one piece of the puzzle for PH-ILD detection.2-4
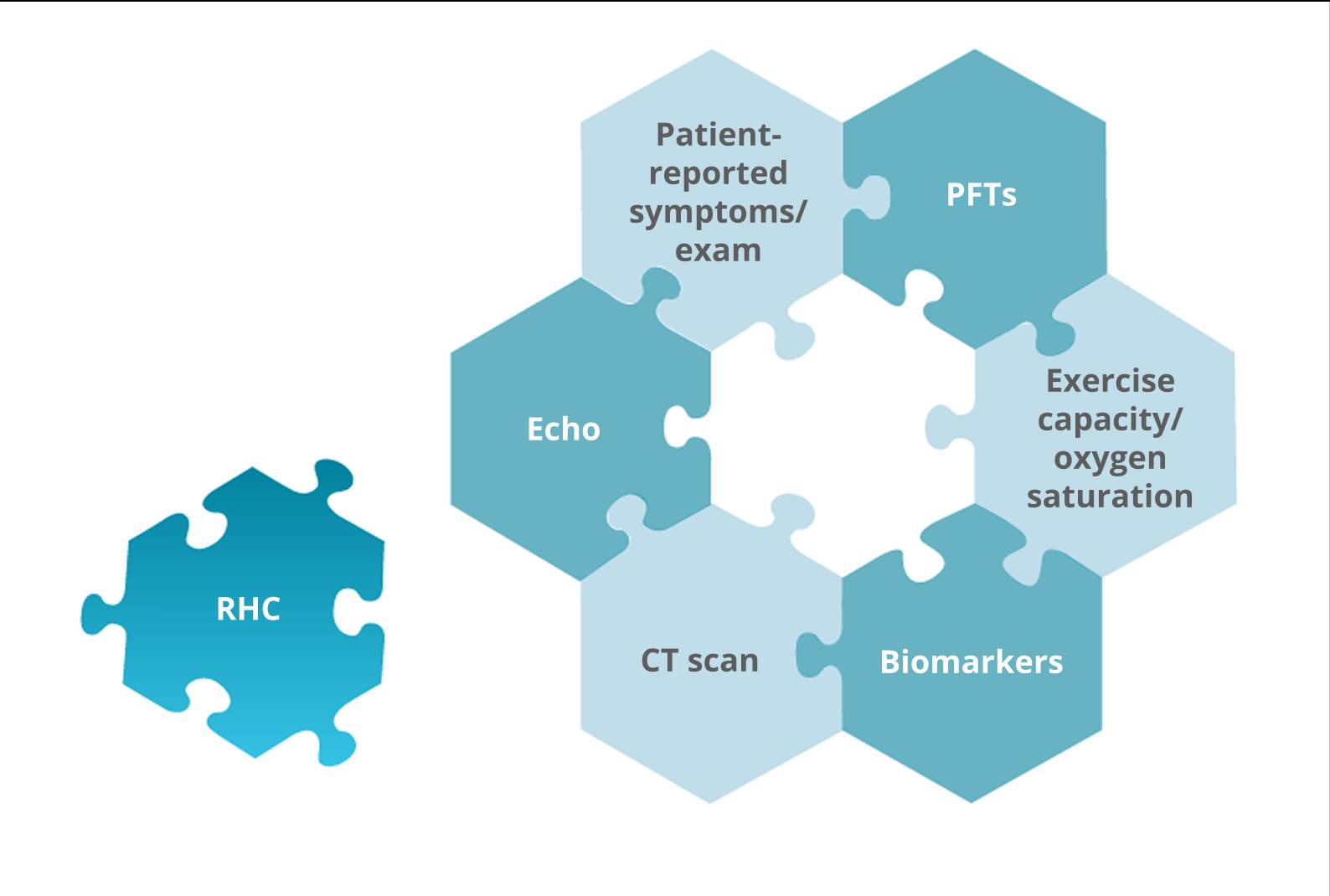
Interpret echo results in conjunction with other clinical findings to help determine the need for RHC.9‡
*Clinical suspicion was determined following integrated review of all relevant information (ie, physical exam, echo, PFTs, and other tests where available) by an expert PH physician.3
†Probability was determined based on modified 2015 ESC/ERS screening recommendations (ie, using peak TRV thresholds plus the presence of RV dilatation and/or dysfunction).
PH was defined as mPAP ≥25 mm Hg. Of the 194 patients with confirmed PH, 140 (72%) had precapillary PH (PCWP ≤15 mm Hg). For the 17 patients misclassified as having a “low probability” of PH, mean mPAP was 35 mm Hg, mean PCWP was 11.4 mm Hg, and mean PVR was 4.9 WU.3
‡Echo-estimated systolic PAP vs RHC-measured systolic PAP.4,6
CT=computed tomography; ERS=European Respiratory Society; ESC=European Society of Cardiology; ILD=interstitial lung disease; mPAP=mean pulmonary arterial pressure; PAP=pulmonary arterial pressure; PCWP=pulmonary capillary wedge pressure; PFT=pulmonary function test; PH=pulmonary hypertension; PVR=pulmonary vascular resistance; RHC=right heart catheterization; RV=right ventricular/right ventricle; RVSP=right ventricular systolic pressure; TR=tricuspid regurgitation; TRV=tricuspid regurgitation velocity; WU=Wood units.
The information contained in this section of the site is clinical in nature and specifically created for healthcare professionals. If you are not a US healthcare professional, please click CLOSE to return to the consumer section of the site.

