PH symptoms can be similar to those of ILD, making them hard to distinguish from ILD based on physical examination.1
SCREENING
ILD symptoms can mask the symptoms of PH-ILD1
A recent study showed physical examinations could not be depended upon for accurately predicting and finding PH. By the time signs are visible, it is most often late-stage PH.1
Test results may identify indicators of PH in your patients with ILD, such as1,2:
SIGNS AND SYMPTOMS OUT OF PROPORTION TO LUNG DISEASE
SIGNS OF RIGHT HEART STRAIN/
Uncover PH-ILD early by screening at diagnosis of ILD, as well as regularly screening ILD patients at follow-up visits.
Start early and regular screening of patients with ILD to identify PH before it impacts prognosis
The results of tests you may already be performing can help stratify the risk for PH in patients with ILD. Consider the following recommendations, which include those provided by the 2018 World Symposium on Pulmonary Hypertension1-8*:
Suspect
Suspect PH-ILD when patient
presents with:
Supplemental oxygen needs3
Signs and symptoms out of proportion to lung disease1-3
-
PFT results
- FVC/D LCOratio >1.6
- D LCO<40%
-
6MWT results
- Worsening 6MWD
- Excessive desaturation or dyspnea
Signs of right ventricular strain or failure1-5
- Elevated BNP or NT-proBNP
-
Enlarged PA or RV on CT
- PA:A ratio >0.9
Support
Support your suspicion of PH-ILD with:
Echocardiogram1,2,5,6
- Elevated RVSP (>40 mm Hg)
- Signs of right ventricular dysfunction
Confirm
Confirm PH-ILD with:
Right heart catheterization (RHC)2
Hemodynamic definition7,8†
- mPAP ≥25 mm Hg‡
- PAWP ≤15 mm Hg
- PVR >3 WU
*United Therapeutics does not provide medical advice.
† WSPH 2018 recommended an update to the diagnostic criteria for all precapillary PH (mPAP >20 mm Hg, PAWP ≤15 mm Hg, and PVR ≥3 WU [at rest]).7
‡ About half of patients who have both IPF and PH have slightly elevated mPAP of 25-30 mm Hg.1
6MWT results can predict PH and assess functional impairment in patients with ILD such as IPF1
Conducting a 6MWT can help you uncover indicators that may signal your patients with IPF are being affected by PH, including1,3,9:
The 6MWT has broad utility in clinical practice for patients with IPF
The 6MWT can also be used to assess the severity of a patient’s functional impairment independent from measures of the physiological impairment (ie, DLCO, FVC)10
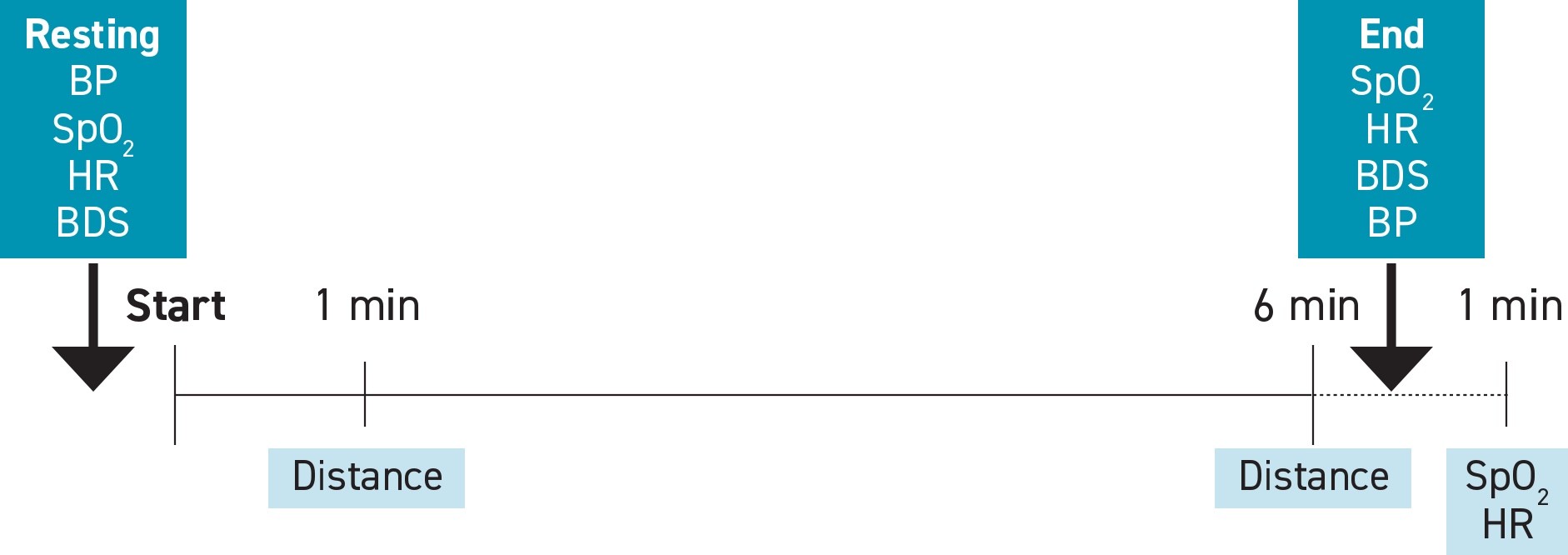
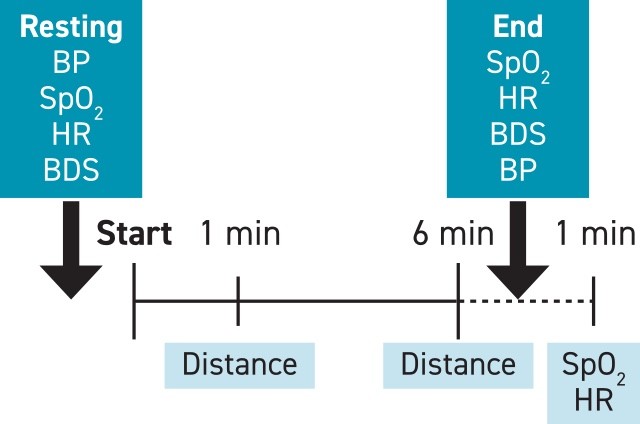
Use a standardized 6MWT format to help ensure assessments are effective and can be reproduced11
Adapted from Lancaster L, et al. Standardization of the 6-min walk test in clinical trials of idiopathic pulmonary fibrosis. Contemp Clin Trials. 2021;100:106227. doi:10.1016/j.cct.2020.106227.
Best practices for the 6MWT11,12
- Use indoor straight course with a hard, flat surface
- ≥30-m (100-ft) course recommended
-
If the patient is on
supplemental
oxygen:
- Give oxygen at the patient’s standard flow rate
- Use the same method for carrying oxygen each time for a specific patient
- Continuously monitor SpO2 and terminate testing if levels drop to <80% for 15 seconds§
- Perform at baseline and subsequent visits
- Use the same patient instructions, timing, and encouragement
§Other reasons for early termination include chest pain, intolerable dyspnea, leg cramps, staggering, diaphoresis, and pale or ashen appearance.11,12
Consistently performing this test will help you identify results that can lead you to suspect PH-ILD.1
Performing tests that can uncover RV dysfunction may help to reveal PH in your patients with ILD1,13:
Elevated NT-proBNP is an important indicator of RV dysfunction14
BNP is secreted by the ventricles in response to volume expansion or pressure overload.15
- NT-proBNP is a fragment of the BNP precursor protein15
BNP and NT-proBNP are quantitative biomarkers of cardiac stress and heart failure.13
- Levels correlate to the severity of cardiac stress and begin to increase before symptoms of severe PH and heart failure (eg, peripheral edema, weight gain) are present13
Increasing plasma levels of BNP or NT-proBNP can help reveal PH.1,3,16
Echocardiogram findings related to the right heart can reveal several indicators of PH-ILD, and multiple echo measures should be examined1
What to look for
- TR jet velocity >3.4 m/s17∥
- Elevated RVSP (>40 mm Hg)2,5,6
- Increased RV size1
- Interventricular septal flattening16,17
- RA area (>18 cm2)17
- Reduced TAPSE (<1.7 cm2)17
What it means
- RVSP is calculated from TR jet velocity and you may need to ask specifically for that result17
- RVSP alone is not always an accurate predictor of PH; additional measures (such as those listed on the left) should also be reviewed1,2¶
While echocardiography is an excellent noninvasive screening tool for PH, it is no substitute for the accuracy of a RHC, the gold standard. These findings should prompt a RHC to confirm PH.1,2
∥If the peak TR jet velocity is >3.4 m/s, there is a high probability of PH and the presence of other echo signs of PH is not required.17
¶TR jet may over/underestimate RVSP in individual patients and may be hard to visualize in patients with chronic lung disease. In addition, some echo findings that are suggestive of PH require expert echo assessment and may not be routinely evaluated.1,2,16,18
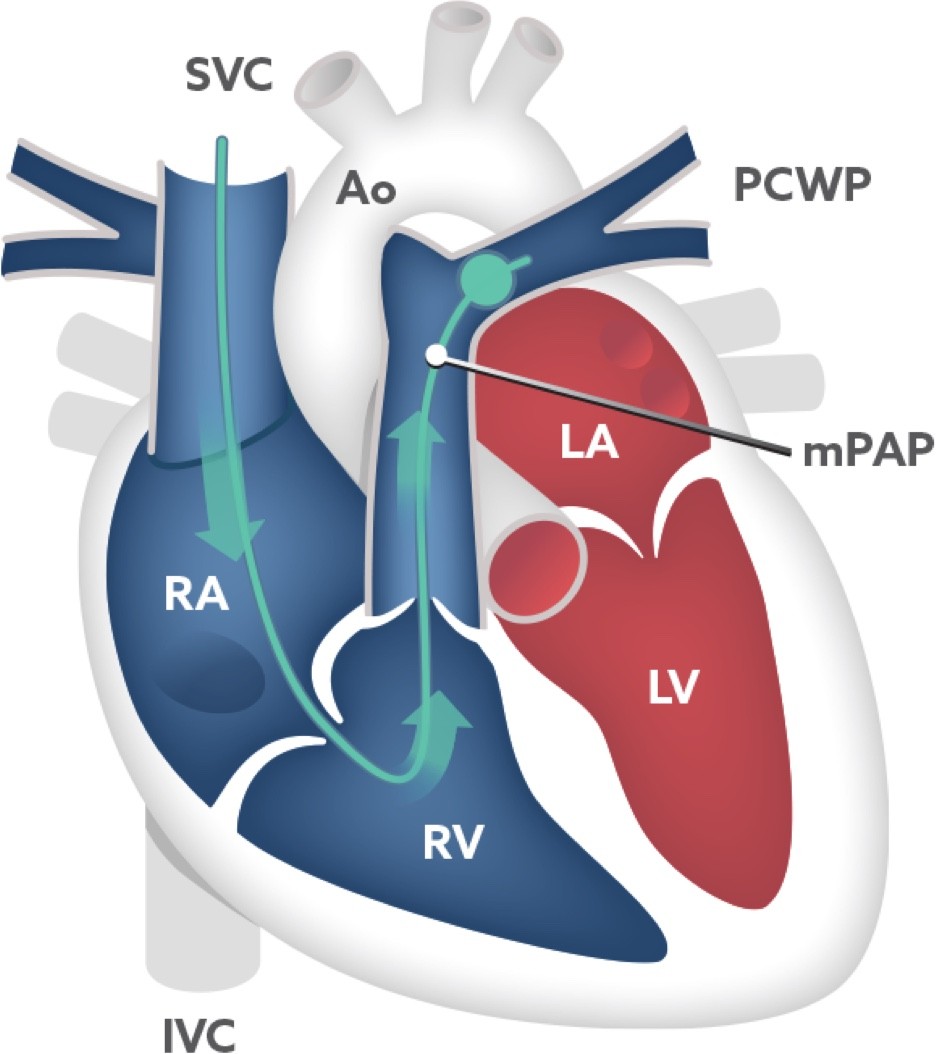
PH is confirmed using hemodynamics obtained via right heart catheterization (RHC)19
RHC is the gold standard for formally diagnosing PH, because it provides a direct measure of hemodynamics19
Allaying concerns about sending a patient with ILD for RHC:
-
There are few contraindications19
- Absolute: right-sided endocarditis, tumor, or thrombus
- Relative: severe coagulopathy or bleeding diathesis
- In fact, even lung transplant candidates are commonly required to have a RHC16
- Low prevalence of serious adverse events/complications (1.1%)20
- Used to diagnose several other conditions19
During the procedure, a catheter is:
- Inserted through the groin (femoral vein), neck (jugular vein), or arm (cephalic vein)
- Advanced into the right atrium using fluoroscopy
- Advanced into the right ventricle
- Advanced into the pulmonary artery to wedge position** and balloon is inflated to measure PAWP/PCWP, a surrogate of left atrial pressure
- Withdrawn back into the pulmonary artery to measure pressure (mPAP), a blood sample is taken to measure SvO2, and cardiac output is assessed with thermodilution or Fick method
**A branch of the pulmonary artery.
RHC is the only way to confirm PH in your patients with ILD. When other results lead you to suspect PH-ILD, order a RHC to confirm the diagnosis.2
Start early and regular screening of patients with ILD to identify PH before it impacts prognosis.
6MWD=6-minute walk distance; 6MWT=6-minute walk test; Ao=aorta; ATS=American Thoracic Society; BDS=Borg dyspnea score; BNP=B-type natriuretic peptide; BP=blood pressure; bpm=beats per minute; CT=computed tomography; DLCO =diffusing capacity of the lung for carbon monoxide; ERS=European Respiratory Society; FVC=forced vital capacity; HR=heart rate; ILD=interstitial lung disease; IPF=idiopathic pulmonary fibrosis; IVC=inferior vena cava; LA=left atrium; LV=left ventricle; mPAP=mean pulmonary arterial pressure; NT-proBNP=N-terminal pro−B-type natriuretic peptide; PA=pulmonary artery; PA:A=pulmonary artery to aorta; PAWP=pulmonary arterial wedge pressure; PCWP=pulmonary capillary wedge pressure; PFT=pulmonary function test; PH=pulmonary hypertension; PVR=pulmonary vascular resistance; RA=right atrium; RV=right ventricular/right ventricle; RVSP=right ventricular systolic pressure; SpO2 =saturation of peripheral capillary oxygenation; SVC=superior vena cava; SvO2=mixed venous oxygen saturation; TAPSE=tricuspid annular plane systolic excursion; TR=tricuspid regurgitation; WSPH=World Symposium on Pulmonary Hypertension; WU=Wood units.
The information contained in this section of the site is clinical in nature and specifically created for healthcare professionals. If you are not a US healthcare professional, please click CLOSE to return to the consumer section of the site.